In the 1990s – when I started my PhD – this was a relevant and intensely debated question. Now, almost 35 years later, we finally have the answer.
It all started with a Boston-based study published in the New England Journal of Medicine in 1987. ICU patients on the ventilator frequently developed gastric bleedings (stress ulcers) and stress ulcer prophylaxis was indicated. In those days the options were antacids or Histamine type 2-receptor (H2-) blockers (ranitidine), both of which aimed to reduce intragastric acidity. However, with less acid in the stomach, bacteria grow better and then aspiration leads to pneumonia; the gastropulmonary route of infection.
Sucralfate protects the gastric mucosa without changing intragastric acidity. In an open-label randomised controlled trial, 130 patients received either sucralfate (n = 61) or antacids, H2- blockers, or both (n = 69). Patients on sucralfate more frequently had gastric aspirates with pH ≤4 (P<0.001), and less Gram-negative bacilli (P<0.05) in gastric, pharyngeal and tracheal aspirates. The incidence of pneumonia was twice as high in the antacid–H2 group (23,2% versus 11.5%, 95% CI 0.89 to 4.58; P = 0.11). “Although results fell just short of statistical significance when analyzed according to intention to treat, they suggest that agents that elevate gastric pH increase the risk of nosocomial pneumonia by favoring gastric colonization with gram-negative bacilli.”
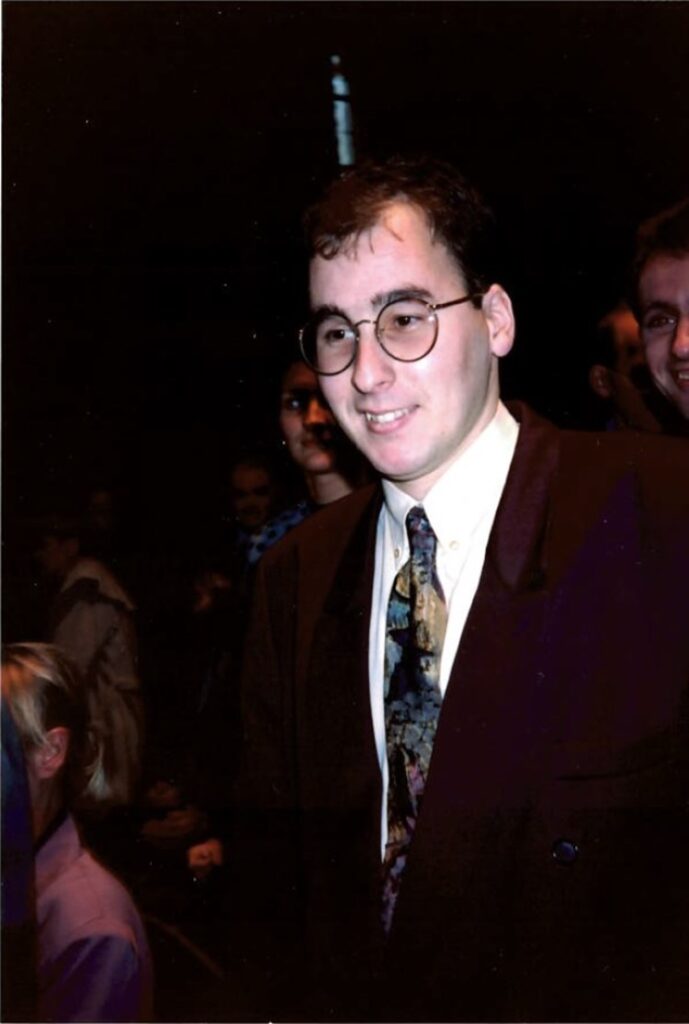
My PhD studies, however, failed to demonstrate an important role of this gastropulmonary route in the pathogenesis of ICU-acquired pneumonia. We summarised these findings, which was accompanied by a contra-editorial of two senior scientists in the field (one from Boston) stating: “In spite of a wealth of data supporting the gastropulmonary hypothesis, Bonten et al have concluded that this route is a largely unimportant source of pneumonia in hospitalized patients particularly those who are intubated.”
The years went by, H2-blockers, antacids and sucralfate were replaced by the more potent proton-pump inhibitors, and the gastropulmonary route issue remained unresolved. The most definitive answer could come from a randomised comparison of PPI to placebo.
And then last week in the NEJM and NEJM Evidence: In a Canadian trial 4,821 patients underwent randomisation in 68 ICUs to either pentazole or placebo. Incidence of Ventilator-Associated Pneumonia was 23,2% and 23,8% yielding a Hazard ratio of 1,00 (95% CI 0,89-1,12). In a meta-analysis of 8 RCTs comparing PPI’s to placebo or no prophylaxis with 8,949 patients it was concluded “that PPI appear to have no effect on pneumonia”; RR 1.00 (95% CI 0.92 to 1.09).
Those two former senior scientists in the field would have to admit that: “With a wealth of data not supporting the gastropulmonary hypothesis, some rightly concluded 25 years ago that this route is a largely unimportant source of pneumonia in hospitalized patients particularly those who are intubated.”

