Today – on paper – in the New England Journal of Medicine an impressive French investigator-initiated, multicenter, double-blind, randomized, placebo-controlled study evaluating the effects of nebulized amikacin on the occurrence of ventilator-associated pneumonia (VAP). This brought back old memories and a reminder that science moves slowly.
A long time ago (previous century!) I did a PhD on just this topic, prevention of VAP. Part of my thesis was a review entitled “Problems in diagnosing nosocomial pneumonia in mechanically ventilated patients” (Crit Care Med 1994; 22: 1683-91). The problem: VAP was diagnosed upon several clinical criteria (fever, leukocytosis), abnormalities on chest X-ray and microbiological culture results from endotracheal aspirates. Each – and even in combination – had low specificity for VAP; implying many false-positive diagnoses, overestimation of incidence, and unnecessary antibiotic use. Moreover, an intervention that would result in negative culture results would also reduce the incidence of VAP, regardless of clinical symptoms.
The possible solution was invasive diagnostics – bronchoscopy to obtain samples from deep inside the lungs (instead of the upper endotracheal part) combined with quantitative cultures. Famous French investigators, Jean-Yves Fagon and Jean Chastre, demonstrated that this approach reduced the incidence of VAP by 50% without affecting patient outcome. Yet the invasive approach did not survive due to the fear of missing out (sensitivity may not be 100%) and the hassle of performing bronchoscopy. So-called deep non-bronchoscopic endotracheal aspirates became the standard.
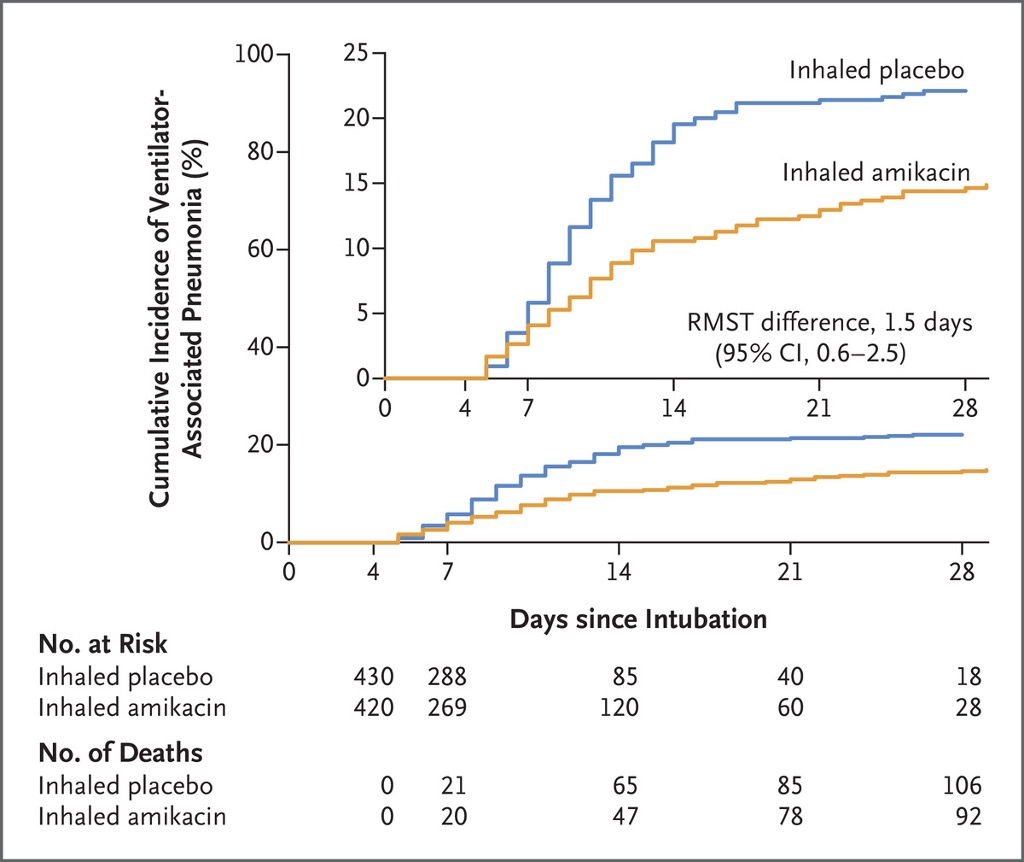
Now, in this study with nebulized amikacin, VAP was diagnosed upon “a positive quantitative bacterial culture in a pulmonary sample and at least two of the following findings: hyperleukocytosis, leukopenia, fever, or purulent secretions with a new infiltrate on a chest radiograph”. There is no information on how these pulmonary samples were obtained. The protective effect of nebulization (which was used for 3 days only) started immediately, as can be seen from the incidence curves for both groups.
Therefore, the possibility of artificial sterilization of microbiological cultures through nebulized amikacin is not excluded. This could have been mentioned as a study limitation and makes me realize that – after 30 years – the problems in diagnosing pneumonia in these patients still have not been solved.

