Last week, ECDC issued a risk assessment on the emergence of hypervirulent Klebsiella pneumoniae ST23 carrying carbapenemase genes in Europe, concluding that “there is a possibility of potentially untreatable infections in previously healthy adults”.
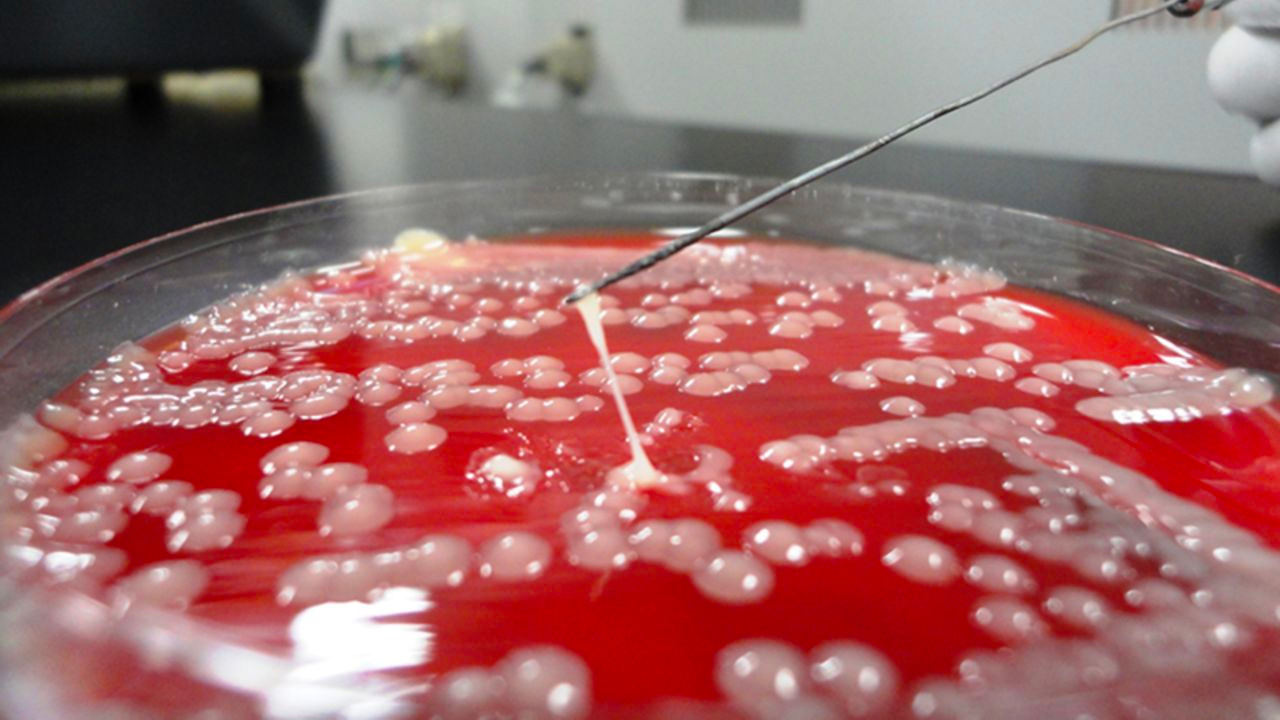
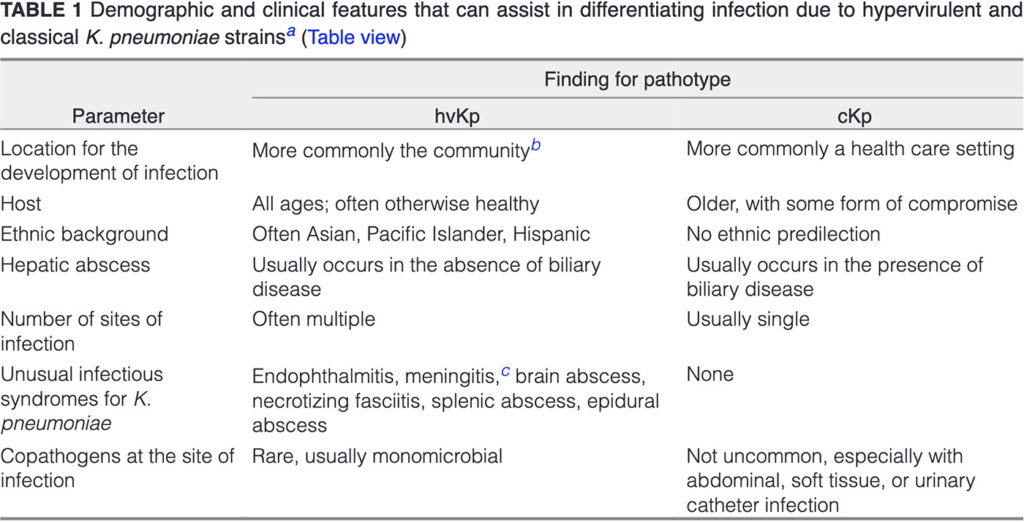
The problem in an overly simplified nutshell: There are 2 types of Klebsiella; (1) The Asian variant characterized by severe infections in healthy individuals such as hepatic abscess (hypervirulent, hv), recognizable in the lab as being hypermucoviscous and usually susceptible to standard antibiotics, named hvKp ST23; and (2) the common Klebsiella variants characterized by less severe infections in vulnerable individuals (mostly in healthcare settings), frequently and increasingly resistant to antibiotics, named “common Kp”, or cKp. See the table below taken from here.
Now there is an increase in hvKp ST23 strains coming from multiple countries outside Asia and being resistant to carbapenems. ECDC lists five clusters of this hvKp ST23-K1 lineage, and the largest comes from Ireland (74 of 93 isolates). Since 2019, there has been “transmission in a network of healthcare facilities including acute care hospitals and residential facilities in the south-east of Ireland with sporadic related cases in other regions likely related to patient transfer.” The clinical characteristics of 23 patients in this outbreak have been described and four were infected, all others were colonized. All four infected patients had community-acquired infections; three had bloodstream infection (from biliary sepsis, urosepsis and unknown origin) and one had UTI.
Identification of hvKp ST23-K1 carriage mostly results from targeted screening for carbapenem-resistance, and the emergence mostly comes from carriage in patients with healthcare exposure: It thus seems that the community-based hvKp ST23-K1 has found a new niche in vulnerable patients in healthcare settings and – along the way – has picked up carbapenem resistance. Yet, it might be that – along the way – this hypervirulent strain has lost its hypervirulence, and transformed into a “common” Klebsiella phenotype, mostly colonizing hospitalized patients. Like an unnamed Dutch politician: after 20 years of humiliating minorities, he is suddenly becoming an acceptable son-in-law.
The emergence of hvKp ST23-K1 definitely deserves our attention. Well-designed epidemiological studies are now needed to determine its clinical relevance. Within the Ecraid network, two studies are enrolling patients at risk for such infections: POS-VAP and POS-cUTI. The teams are now analyzing the data to see if and how often hvKp ST23-K1 caused infection.
Featured photo: BMJ