That’s a question I’ve asked myself many times. If it doesn’t, antibiotics would not be needed, attributable mortality would be absent, and VAP prevention would not increase survival. A new – and excellent – study in Lancet Respiratory Medicine provides new evidence that fits my pre-opinionated and unproven belief.
In the REGARD-VAP study Mo Yin and colleagues randomized patients with VAP and beneficial clinical response (lower body temperature and hemodynamic stability) after two days of antibiotic therapy to a total duration of six or 14 days (=usual care) of antibiotics. In 39 ICUs in Nepal, Thailand and Singapore, 461 patients were randomized in which VAP was diagnosed upon clinical and radiographical criteria without biomarker testing or bronchoscopy. The primary endpoint was a composite of death or recurrent pneumonia within 60 days, assuming that this would occur in 55% of those with usual care and with a non-inferiority margin of 12%. In the intention-to-treat population the primary endpoint was met in 41% in the short-course group compared to 44% in the usual care group: absolute risk difference –3% [one-sided 95% CI –∞ to 5%], clearly non-inferior.
Both groups really differed in antibiotic exposure:
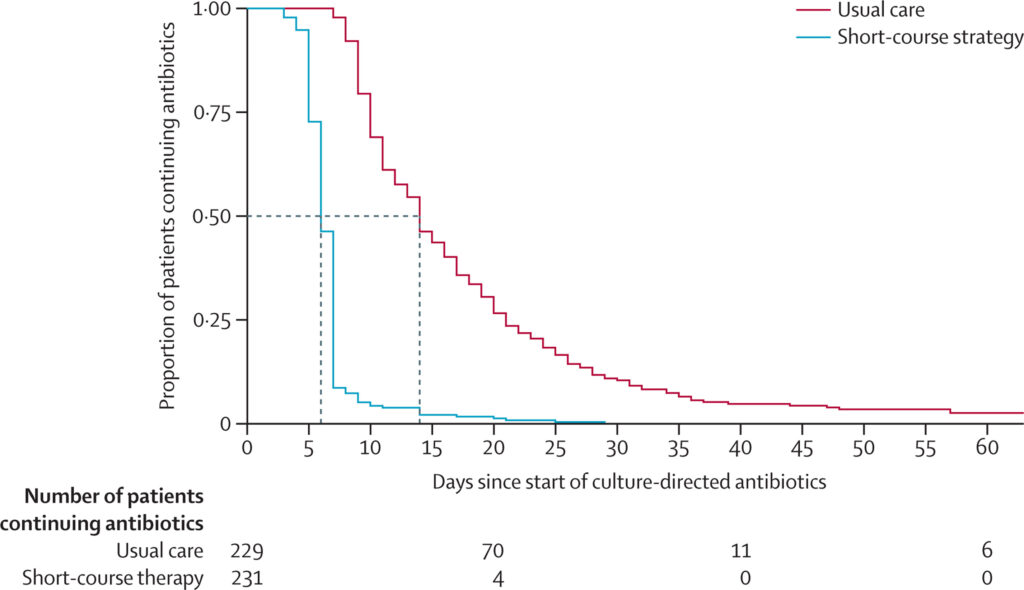
Dotted lines represent median duration of antibiotic treatment in each group. VAP=ventilator-associated pneumonia.
This figure made me think of a study I was involved in that was done in the previous century (Denessen et al. AJRRCM 2001; 163: 1371-5). The lower lines reflect the resolution of the clinical parameters in the diagnosis of VAP. Our conclusion then was: “A strategy to treat VAP for 7 instead of 14-21 days should be tested in a prospective randomized study design.” It was actually tested by Chastre and Fagon, but that study did not close the book on the longer treatment (JAMA 2003; 290: 2588–98).

The findings of Mo Yin do not prove that VAP does not exist, and deep down inside I know it probably does. To me, this study – once again – emphasized the need for a reliable diagnosis. Many of those treated for VAP probably don’t have an invasive infection and may not even need antibiotics. A long time ago there was a serious attempt to increase specificity of diagnosing VAP through adding quantitative cultures obtained through bronchoscopy. Incidence of VAP immediately decreased by 50%, without affecting patient outcome. Yet this practice has been abandoned and no other diagnostic criteria have been added.
We once analyzed the timing of VAP occurrence, assuming that ICU physicians don’t wait with administering antibiotics if VAP is diagnosed and taking advantage of the computer-based time-logged antibiotic prescription in our ICU. The risk of VAP peaked at 11am (after viewing chest X-rays) and 1pm (during clinical rounds) and was nearly zero during nightly hours (unpublished data).
A better diagnosis of VAP may allow even less exposure to unnecessary antibiotics and better management for those that really have invasive infection. But the six days is a good starting point.

