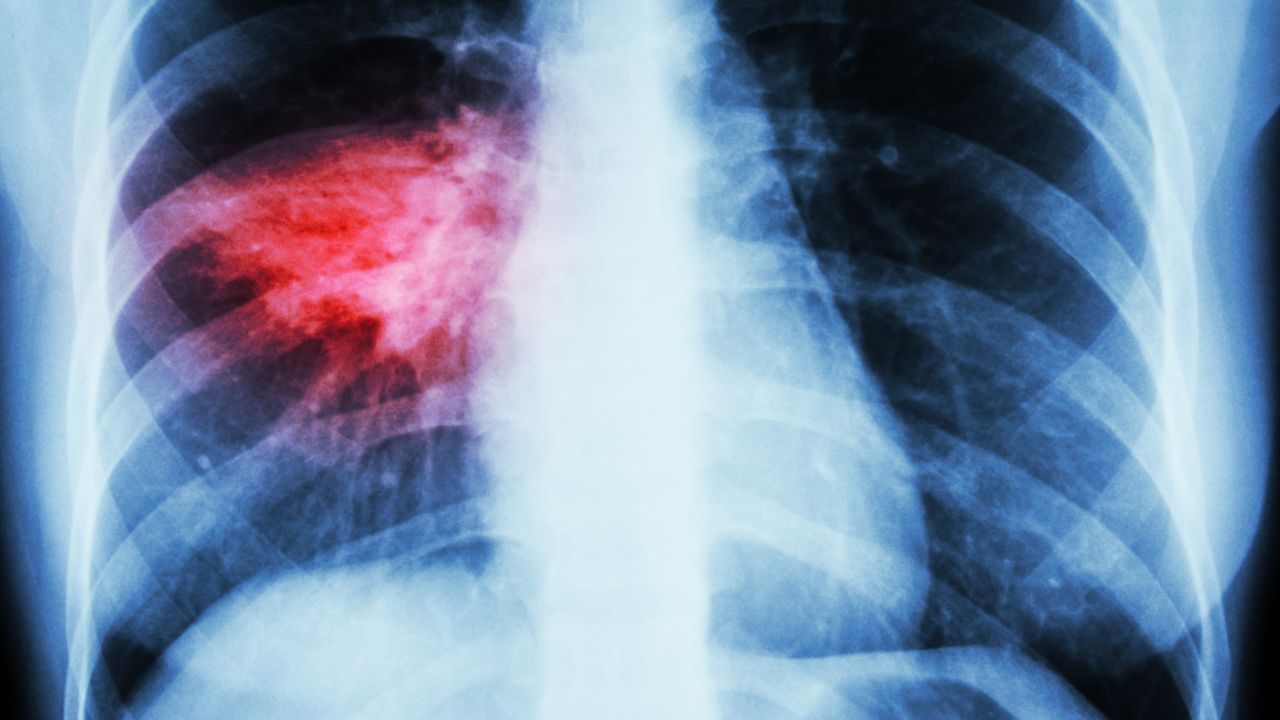
Should patients hospitalized with community-acquired pneumonia (CAP) be treated with macrolides added to a beta-lactam antibiotic? This is a long-lasting discussion.
The rationale for double treatment includes coverage of atypical pathogens in the empiric regimen, as well as immune modulation. Last week, a new piece of evidence was added. The ACCES study is a double-blinded placebo-controlled RCT comparing the effects of oral clarithromycin added to standard of care treatment in patients hospitalized with CAP in Greece. The primary composite endpoint was determined at day four of treatment and included: (1) >50% decrease in respiratory symptom severity score and (2) >30% decrease in SOFA score or ≥80% decrease in procalcitonin from baseline or level <0.25 ng/mL. In two study groups (134 and 133 patients) clarithromycin enhanced early clinical response and cytokine measurements were compatible with more effective reversal of a paralyzed immune response. The study was not powered for survival outcomes, but there was a numerical 3,3% lower day-90 mortality among those who received clarithromycin.
These findings contradict those from a pragmatic open-label cluster-randomized trial conducted in the Netherlands (2011-2013) where three empiric treatment strategies were compared. Motivated deviation from protocol was allowed and all patients hospitalized and treated for presumed CAP were included (25% lacked signs of pneumonia on chest X-ray). In this study, the strategy of preferred beta-lactam monotherapy was – in intention-to-treat and per-protocol analysis – non-inferior to the preferred beta-lactam plus macrolide therapy strategy for day-90 mortality (risk difference -1.9%, 90%CI -0.6-4.4; risk higher in combination therapy periods). In those days, patients still received erythromycin intravenously, which is associated with acute heart failure.
Can we explain the different outcomes from both studies? Both had a (different) randomized approach, but most importantly almost completely different patient populations. The ACCES study patients were older, more severely ill, treated with other antibiotics and day-90 mortality was three times higher than in that in the CAP-START study. This seriously hampers comparing the two studies. See the table below:
| ACCES study (2024) (n=134) | CAP-START (2015) (n=739) | |
| Oral clarithromycin (or azithromycin) | 134 | 388 (iv erythromycin 263) |
| Age | 81.5 (73-87) | 70 (59-80) |
| CURB | 2 (2-3) | 1 (1-2) |
| PSI score | 122 (101-138) | 84.8 (SD27.8) |
| Day-90 mortality | 34% | 11% |
| Other antibiotics | ||
| Amoxicillin or penicillin | 0 | 396 (54%) |
| Amoxicillin/clavulanic acid | 29 (22%) | 354 (48%) |
| 2nd/3rd generation cephalosporin | 54 (40%) | 268 (36%) |
| Ceftazidime | 0 | 21 (3%) |
| Fluoroquinolone | 6 (5%) | 108 (15%) |
| Piperacillin/tazobactam | 49 (37%) | 0 |
| Ceftaroline | 3 (2%) | 0 |
| Meropenem | 6 (5%) | 0 |
| Metronidazole/Clindamycin | 15 (11%) | 0 |
| Glycopeptides | 9 (7%) | 0 |
| Aminoglycoside | 2 (2%) | 0 |
| Linezolid | 11 (8%) | 0 |
Yet, the ACCES study provides strong evidence and rationale to support macrolides as part of standard care treatment. However, its study population may not be generalizable to all-comers with CAP in other/many/most settings. Confirmation of these findings in similar and broader patient populations is needed, preferably with randomized study designs. Macrolides are investigated in REMAP-CAP, randomizing patients admitted in ICU with CAP to either a short or extended course of macrolides in addition to other antibiotics or not. 1200 patients enrolled and counting. No conclusion yet. Joining REMAP-CAP is possible.